- Research
- Open access
- Published:
The faces behind vaccination: unpacking the attitudes, knowledge, and practices of staff of Cameroon’s Expanded program on Immunization
Human Resources for Health volume 21, Article number: 88 (2023)
Abstract
Background
Immunization is regarded as one of the most cost-effective public health interventions in global health. However, its cost-effectiveness depends greatly on the knowledge and skills of vaccinators. With the growing complexity of immunization programs, the need for a well-trained vaccination workforce cannot be overemphasized. In this study, we assessed the knowledge, attitudes, and practices among vaccination staff in Cameroon.
Methods
Through a descriptive cross-sectional design, we used structured questionnaires and observation guides to collect data from vaccination staff in health facilities that were selected by a multistage sampling method. Data were analyzed using STATA 13 software.
Results
Overall, we collected data from Expanded Program on Immunization focal staff in 265 health facilities across 68 health districts. Over half (53%) of the surveyed facilities were found in rural areas. Nearly two-thirds of health facilities had immunization focal staff with knowledge gaps for each of the four basic immunization indicators assessed. In other words, only 37% of staff knew how to estimate coverages, 36% knew how to inteprete the EPI monitoring curve, 35% knew how to prepare vaccine orders, and 37% knew how to estimate vaccine wastage. In terms of practices, staff waited for more than ten children to be present before opening a 20-dose vaccine vial in 63% of health facilities, and more than five children to be present before opening a 10-dose vaccine vial in 80% of surveyed facilities. Provision of vaccine-specific information (informing caregiver about vaccine received, explanation of benefits and potential side effects) during immunization sessions was suboptimal for the most part.
Conclusion
This study suggests marked deficits in immunization knowledge among vaccination staff and exposes common attitudes and practices that could contribute to missed opportunities for vaccination and hinder vaccination coverage and equity in Cameroon. Our findings highlight the urgent need to invest in comprehensive capacity building of vaccination staff in Cameroon, especially now that the immunization program is becoming increasingly complex.
Introduction
Immunization is regarded as one of the most cost-effective public health interventions in modern public health history. This intervention alone averts between 3.5 to 5 million deaths annually [1] and has substantially contributed to the observed reduction in global child mortality, from 12.5 million under-five deaths in 1990 to 5.3 million deaths in 2018 [2]. Over the past decades, great strides have been made globally in expanding the reach of immunization programs; however, the coverage of the third dose of the diphtheria–tetanus–pertussis, containing vaccine (DTP-3) has not gone above 86% since 2018 [3]. Similarly, despite strides in improving the performance of routine vaccinations, coverage in the WHO African region has stagnated for about a decade, with significant inter- and intra-country disparities [4,5,6].
The expanded program of immunization (EPI) in Cameroon, which was launched in 1976, has remarkably contributed to increased vaccination coverage over the past four decades [7]. In 2010, Cameroon was one of the three Central African countries with an immunization coverage rate of over 80% [8]. Despite this remarkable progress, national immunization coverage still falls below set targets. In Cameroon's 2015 to 2019 comprehensive multi-year plan (cMYP), the EPI envisaged raising the DTP-3 coverage from 89% in 2013 to 92% in 2019. Unfortunately, the EPI did not only fail to attain this goal, the program registered a 22 percent point decrease, with DTP-3 coverage plummeting from 89% in 2013 to 67% in 2019 [6, 9]. This drop in immunization coverage has left many children without life-saving vaccines. Indeed, according to the most recent Demographic and Health Survey (DHS) in Cameroon, only 52% of children aged 12–23 months have received all essential vaccinations (one dose of Bacille Calmette-Guerin, BCG and measles vaccines and three doses of DTP and poliomyelitis vaccines) [10]. In addition, in 2019, Cameroon was among the top 10 countries contributing to 86% of the world's 7.3 million estimated zero-dose children [11].
Immunization coverage has been shown to be driven by several factors [12, 13]. Indeed, a well-functioning routine immunization system relies on interactions of several components, including robust cold chain and logistics management systems, sustainable financing, strong managerial and technical leadership, and quality service delivery [14]. In addition, a well-functioning vaccination system with quality vaccination services anchors on effectiveness as a core guiding principle, defined by the World Health Organization as providing evidence-based vaccination services based on scientific rigor to achieve the best possible outcomes [15]. While the community needs to collaborate with healthcare providers to improve coverage, the quality of vaccination services provided by health personnel is imperative for the success of vaccination programs [16]. This success has been shown to significantly depend on the knowledge, attitudes, and skills of vaccination and managerial staff at healthcare facilities [17]. Indeed, the need for a well-trained and competent health workforce for vaccination cannot be overemphasized, particularly in recent years where immunization programs are bent on "leaving no one behind" and expanding the benefits of vaccination to every individual, irrespective of who he/she is and where he/she lives [18]. Meeting this noble goal will require significant improvements in providers' knowledge, attitudes, and practices, as these could positively or negatively influence parental decisions to seek vaccination services or return for subsequent vaccinations. For example, Musa et al. reported increased immunization service utilization in settings where health workers displayed positive attitudes and practices [19]. However, such evidence is limited in sub-Saharan Africa. As a result, evaluating the knowledge, attitudes, and practices of vaccination staff may serve as a standpoint for improving the quality of immunization service delivery, which in turn can improve immunization coverage and equity in many settings.
In Cameroon, several studies have examined specific drivers of declining routine immunization (RI) performance [20,21,22,23,24]. However, none of the work focused on assessing immunization knowledge among vaccination staff and their attitudes and practices during vaccination sessions. Thus, this study aimed to generate preliminary data on this neglected area of immunization.
Materials and methods
Study design
This descriptive cross-sectional study was based on data from a national baseline assessment that was implemented by the EPI in collaboration with the Clinton Health Access Initiative (CHAI). The study aimed at identifying and characterizing potential factors contributing to declining immunization coverage in Cameroon.
Study setting
The study was conducted in Cameroon, a country that is located in the Gulf of Guinea. The country has a population of approximately 28 million inhabitants and a total surface area of 475,440 km2 [25]. The country is divided into ten administrative regions: Adamawa (AD), Center (CE), East (ES), Far-North (EN), Littoral (LT), North (NO), North West (NW), West (OU), South (SU) and South West (SW) regions [26].
Cameroon's health sector is organized into three main levels (central, intermediate, and peripheral), each having specific competencies, administrative, health, and dialogue structures. The health structure lies under the leadership of the Minister of Public Health. The central level is led by various directorates under the leadership of the Minister of Public Health and focuses mainly on developing policies, strategies, and coordination. The intermediate level is led by the 10 Regional Delegates and provides technical support to the 189 health districts nationwide. District Medical Officers manage the health districts at the third level, the operation or implementation level for primary health care in Cameroon. Preventive services, including, immunization activities, are incorporated into all health system levels [27].
Sampling
A multistage sampling technique was used to select health facilities. Before sampling, the total number of districts was allocated proportionately to the total number of districts per region in the ten regions. Then, the number of urban and rural districts was assigned within each region based on the region-specific breakdown and health facilities were allocated across regions in proportion to the national distribution.
The districts were then randomly selected within the specified region's urban or rural strata in the first stage. Health facilities were randomly selected within the identified rural/urban districts in the second stage. This selection was made while ensuring that the same number of facilities was selected within each district.
Study procedures
Administrative approval
Administrative approval was obtained from the ministry of public health before data collection. Additionally, written approvals were also obtained from all regional delegations of public health, who in turn issued administrative letters to district heads requesting full support for the data collection process.
Training
Training was carried out in all regions to provide regional supervisors and data collectors with the necessary knowledge and skills to undertake the baseline assessment. The training consisted of theoretical presentations and practical sessions on data collection, entry, and transmission processes. During practical sessions, assessors were split into groups and accompanied by the assessment management team to health facilities, where they were closely observed as they completed questionnaires and observation guides.
Data collection
Data collection was conducted by trained assessors selected from regional and district staff. The assessment management team and regional EPI teams developed data collection plans for target districts and health facilities. To prevent unproductive visits during data collection (e.g., visiting a health facility when there was no vaccination session), assessors contacted the health facilities via phone to remind them of planned visits. Upon arrival in the facilities, the purpose of the assessment was explained to the facility head or their representative. Then the assessor first obtained informed written consent before proceeding to interview the health provider in charge of immunization service delivery in each facility and observed an ongoing fixed post-vaccination session.
Study tools
The tools used for this study were:
-
A health facility questionnaire designed to assess the knowledge, attitudes and practices of immunization staff and their knowledge of key immunization indicators.
-
Vaccination Services Observation Guide, which included several prompts to assess the attitudes and practices of vaccinators during immunization sessions.
These study tools were developed in English and French and pre-tested in four facilities in Yaounde prior to study initiation.
Data management and analysis
Before data entry, a comprehensive database was built, pre-tested, and validated by an expert data manager. Each assessor entered data from the filled questionnaires and observation forms into the database and transmitted the files to a secure server within three days of data collection. Data were exported and cleaned in Microsoft Excel 2016 and analyzed with STATA 13 software (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP). Frequencies and proportions were used to summarize variables of interest, and the unit of analysis was the health facility. Districts and facilities were sampled proportional to national distributions, and no post-stratification weights were applied.
Operational definition of variables
Immunization staff knowledge: This was defined as the knowledge of the health provider in charge of immunization service delivery (EPI focal point) on four key immunization indicators (vaccination coverage estimation, Interpretation of the EPI curve, preparation of a vaccine order, and estimation of vaccine wastage). Knowledge on each of these indicators was assessed separately, as either correct or incorrect based on EPI recommendations.
Immunization staff attitudes and practices: This was based on assessors' observation during fixed post-immunization sessions and the responses from the EPI focal point's interview.
Immunization staff: Included all health staff working in the immunization unit. Only the head of the immunization unit (or their representative) was interviewed for knowledge assessment.
Results
General characteristics of health facilities
A total of 265 health facilities in 68 health districts were assessed nationwide during the study period. Over half (53%) of the facilities were in rural areas. Of all the facilities surveyed, the Center (21%), Littoral (13%), and North West (13%) regions were most represented, as shown in Table 1.
The majority (84%) of the health facilities had two or more staff assigned to the immunization service unit, though with notable regional disparities. Notably, in the South region, 31% of health facilities had only one health provider assigned to vaccination services. Over two-thirds (93%) of the facilities had no trained immunization staff, with facilities in the South (85%) and East (100%) having very high proportions of untrained staff.
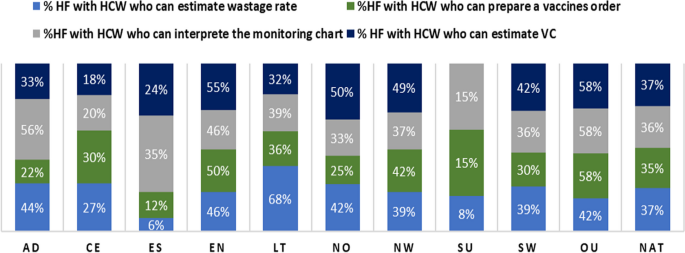
Vaccine-provider knowledge on key immunization indicators
Figure 1 provides level of awareness of selected immunization indicators. Overall, only 37% of health facilities had immunization staff who knew how to estimate vaccination coverage. In most regions, less than a third of health facilities had staff knowledgeable on vaccination coverage estimation. It is worth noting that in the South region, no surveyed facility had staff who had knowledge on estimating vaccination coverage. Figure 1 also shows that at national level, only 36% of health facilities had staff who could interpret the EPI monitoring curve, with the West (58%) and Adamawa (56%) regions having the highest proportion of such staff. It was also noted that only 35% and 37% of health facilities had staff knowledgeable on preparing a vaccination order and estimating vaccine wastage, respectively (Fig. 1).
Healthcare workers attitudes and practices
Table 2 provides a battery of attitudes and practices of immunization staff that were observed by study staff during immunization sessions in the 265 surveyed facilities. In terms of vaccine handling and utilization, HCWs in 46% of facilities waited for 10 to 15 children to be present for vaccination sessions before a 20-dose BCG vial was opened, while in 17% of facilities, staff waited for more than 15 children to be present. Similarly, in 68% of health facilities, HCWs waited for five to nine children to be present before opening a 10-dose pentavalent or measles vaccine vial, while 21% of facilities waited for at least nine children before opening a 10-dose vial. In all facilities in the Far North and North regions, HCW did not open a vial if less than 5 children were present for vaccination.
Practices regarding handling of multi-dose vials were concerning. Overall, HCW in 18% of the surveyed facilities noted the date that a WHO-MDVP was opened—an observation that was consistent across all 10 regions (Table 2). Another harmful practice was placing vials on icepacks. Indeed, in 44% of surveyed facilities, HCWs placed vials on ice packs during immunization sessions, and this practice was particularly prominent in the North (65%), Center (55%), Far North (54%) and East (53%) regions.
Table 2 also illustrates some key parameters that were checked by HCW before vaccine administration. As illustrated, HCW in 94% of surveyed facilities verified the ages of children before administering a vaccine—a finding that was consistent across the 10 regions. Similarly, HCWs in nearly 90% of facilities verified the vaccines that the child had previously received before administering the next one. Despite these positive practices, HCW in 49% of health facilities, did not inform caregivers about the vaccine their child was receiving. Similarly, HCW in 51% of surveyed health facilities did not educate caregivers about the benefits of vaccination. Similarly, HCWs did not inform the caregivers about normal and potential side effects of vaccination in 68% and 69% of surveyed facilities, respectively. Last, but not least, HCWs in 14% of facilities did not request caregivers to return for follow-up vaccinations.
Discussion
This study, which was nested in a national baseline assessment of Cameroon's immunization system, aimed at examining the immunization knowledge of vaccination staff in Cameroon as well as their attitudes and practices during vaccination sessions. We found that the knowledge of immunization staff on vaccination in practice was limited, with remarkable regional disparities. In assessing staff attitudes and practices during vaccination sessions, we noted significant gaps in health worker-to-caregiver communication and the utilization and handling of multi-dose vaccines. To the best of our knowledge, this is the first study evaluating immunization staff's knowledge, attitudes, and practices on a national scale in Cameroon.
We found that for the four basic immunization indicators assessed (vaccination coverage estimation, EPI monitoring chart interpretation, vaccine order preparation, and vaccine wastage estimation), nearly two-thirds of health facilities had focal immunization staff with suboptimal knowledge. This observation corroborates the findings of a study carried out in one district in Cameroon, which noted limited vaccination knowledge of health personnel using a different set of immunization indicators [16]. Another study in Nigeria reported that only 55% of vaccinators in 54 surveyed facilities were familiar with WHO-MDVP for minimizing vaccine wastage [28]. A poor knowledge base could limit immunization staff's ability to plan and deliver quality vaccination services, thus hindering improvement in vaccination coverage. One of the factors that could be at the root of this knowledge deficit in our study is the limited capacity building of staff working in vaccination services, as up to 67% of the surveyed facilities had no staff trained on immunization. This issue highlights the need for regular capacity building of the vaccination workforce as immunization programs become more complex with the increasing number of vaccines and recommendations [14]. Training programs have been shown, in different settings, to increase the knowledge of primary care health workers involved in vaccination and improve vaccination coverage [29, 30].
As pertains to the utilization of multi-dose vaccines, vaccine providers waited for more than 10 children to be present before opening 20-dose vaccine vials in over three-quarters (75%) of health facilities, and more than 5 children to be present before opening 10-dose vaccine vials in a great majority (91%) of surveyed facilities. This practice is comparable to findings from a study in Nigeria which found that, on average, vaccinators waited for a minimum of six children to be present before opening a 10-dose measles-containing vaccine (MCV) [28]. Similarly, in a multi-country qualitative study, some healthcare workers in Senegal and Zambia reported sending unvaccinated children back home because not enough children were present to necessitate the opening of a new 10-dose vial [31]. These attitudes and practices with multi-dose vaccines could lead to increased caregiver waiting time, influencing their decisions for future vaccinations, and contribute to missed opportunities for vaccination (MOV) either directly or indirectly, which in turn may impact vaccination coverage [32]. Mindful that the objective usually driving these practices is to minimize vaccine wastage and prevent stockouts, these findings underscore the need to put policies and strategies in place to ensure reducing MOV is prioritized over wastage concerns [30]. As a result, many countries are considering switching to products with smaller dose vials; however, such a switch could overwhelm the cold chain and supply chain capacity of the vaccination system and significantly increase the cost of vaccination per child [33]. This finding was even more surprising for vaccine products that meet the four critical criteria for the WHO Multi-Dose Vial Policy that allows for the storage of open vials for up to 28 days [34]. However, this could be accounted for by high staff attrition, particularly in private facilities in urban areas—further highlighting the importance of putting in place a system for continuous learning, including onboarding, e-learning, coaching, and supportive supervision.
Another remarkable finding was that vaccine providers placed vials on ice packs during vaccination sessions in nearly half (44%) of health facilities. This practice could compromise the potency of freeze-sensitive vaccines. Exposure of vaccines to negative temperature is pervasive in Cameroon, not only limited to immunization sessions but across the entire supply chain, from central vaccine stores to outreaches [23]. Again, this is a capacity issue that should be corrected with training to improve their vaccine handling knowledge and practices.
We also found that providing vaccine-specific information (informing caregiver about vaccine received, explanation of benefits and potential side effects) during immunization sessions was suboptimal for the most part. Our findings are discordant with that of Al-Salihi et al. in Iraq, who reported that up to 96% of primary healthcare staff informed caregivers about potential side effects during vaccination sessions [35]. This difference could be because up to 87% of immunization staff received at least one formal training course on vaccination, unlike in our study, where over two-thirds of surveyed facilities (67%) had no staff trained on immunization. A vast majority of caregivers consider health workers as their primary source of immunization information, and their recommendations are known to influence parental decisions [14, 36, 37]. Vaccination sessions offer a unique opportunity to interact with health workers and gain basic vaccine-specific information. However, immunization staff commonly need more training on interpersonal skills and their contribution to improving vaccination uptake [14].
While our study has revealed significant gaps in the knowledge, attitudes and practices of immunization staff in Cameroon, certain limitations must be considered while interpreting our results. First, the data collected from observation sessions may have been subject to some bias because EPI personnel were aware of being observed and may have performed differently from a regular unobserved day. Secondly, the knowledge indicators assessed were not comprehensive as this was done in the context of a larger assessment, narrowing the extent of the knowledge assessment. Last, but not least, given that the unit of analysis was the health facility, individual provider level variations present at facility level could have been missed. However, the nationwide coverage of our study increases the generalizability of our study findings and highlights specific regional deficits in vaccination workforce knowledge, attitudes and practices.
Conclusion
This study highlights marked deficiencies in immunization staff training and knowledge of basic EPI indicators. It also exposes several gaps in knowledge, attitudes and practices in vaccine handling, utilization, and caregiver information sharing that could contribute to MOV, which may impact vaccination coverage and equity in Cameroon. This challenge prompts a great need to invest in systematic, comprehensive capacity building of immunization staff in Cameroon while strengthening supportive supervision and formulation of policies and strategies to minimize vaccine wastage without creating MOV.
Availability of data and materials
Data used for this research are available from the corresponding author upon reasonable request.
Abbreviations
- CHAI:
-
Clinton Health Access Initiative
- EPI:
-
Expanded Program on Immunization
- HCW:
-
Healthcare workers
- HF:
-
Health facility
- MCV:
-
Measles containing vaccine
- MOV:
-
Missed Opportunities for Vaccination
- WHO-MDVP:
-
WHO Multi-dose Vaccine Policy
References
World Health Organisation. Vaccines and immunization [Internet]. 2022 [cited 2022 Dec 29]. Available from: https://www.who.int/health-topics/vaccines-and-immunization.
United Nations Children’s Fund (UNICEF). Levels & Trends in Child Mortality: Report 2019, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation (UN IGME). New York; 2019.
World Health Organisation. Global Vaccine Action Plan 2011–2020. 2013.
Okeibunor JC, Akanmori BD, Balcha GM, Mihigo R, Vaz RM, Nshimirimana D. Enhancing access to immunization services and exploiting the benefits of recent innovations in the African region. Vaccine. 2013;31(37):3772–6.
Mihigo R, Okeibunor J, Anya B, Mkanda P, Zawaira F. Challenges of immunization in the African Region. Pan Afr Med J. 2017;27(Suppl 3):12.
World Health Organisation. Diphtheria tetanus toxoid and pertussis (DTP3) immunization coverage among 1-year-olds, Global Health Observatory. Available from: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/diphtheria-tetanus-toxoid-and-pertussis-(dtp3)-immunization-coverage-among-1-year-olds-(-).
Programme Elargie de Vaccination(PEV), Ministère de la Santé, Cameroon. PEV :: Historiques. Available from: https://pevcameroon.cm/apropos/histories.
LaFond A, Kanagat N, Steinglass R, Fields R, Sequeira J, Mookherji S. Drivers of routine immunization coverage improvement in Africa: findings from district-level case studies. Health Policy Plan. 2015;30(3):298–308.
Programme Elargie de Vaccination (PEV), Ministère de la Santé, Cameroon. Plan Pluriannuel Complet 2015–2019. 2014. Available from: https://extranet.who.int/countryplanningcycles/file-repository/CMR.
National Institute of Statistics (Cameroon) and ICF. 2018 Cameroon DHS Summary Report. Maryland; 2020. Available from: www.DHSprogram.com.
World Health Organization. Regional Office for Africa. Framework for the implementation of the immunization agenda 2030 in the WHO African Region: report of the Secretariat. 2021.
Bobo JK, Gale JL, Thapa PB, Wassilak SG. Risk factors for delayed immunization in a random sample of 1163 children from Oregon and Washington. Pediatrics. 1993;91(2):308–14.
Biset G, Woday A, Mihret S, Tsihay M. Full immunization coverage and associated factors among children age 12–23 months in Ethiopia: systematic review and meta-analysis of observational studies. Hum Vaccin Immunother. 2021;17(7):2326–35.
Shen AK, Fields R, McQuestion M. The future of routine immunization in the developing world: challenges and opportunities. Glob Health Sci Pract. 2014;2(4):381–94.
World Health Organisation. Quality immunization services: a planning guide. 2022.
EbileAkoh W, Ateudjieu J, Nouetchognou JS, Yakum MN, DjoumaNembot F, NafackSonkeng S, et al. The expanded program on immunization service delivery in the Dschang health district, west region of Cameroon: a cross sectional survey. BMC Public Health. 2016;16(1):801.
World Health Organisation. Global Routine Immunization Strategies and Practices (GRISP): a companion document to the Global Vaccine Action Plan (GVAP). 2016.
Gavi, The Vaccine Alliance. New 2021–2025 high level strategy to leave no-one behind with immunisation approved by Gavi Board. 2022. Available from: https://www.gavi.org/news/media-room/new-2021-2025-high-level-strategy-leave-no-one-behind-immunisation-approved-gavi.
Musa S, Skrijelj V, Kulo A, Habersaat KB, Smjecanin M, Primorac E, et al. Identifying barriers and drivers to vaccination: a qualitative interview study with health workers in the Federation of Bosnia and Herzegovina. Vaccine. 2020;38(8):1906–14.
Russo G, Miglietta A, Pezzotti P, Biguioh RM, BoutingMayaka G, Sobze MS, et al. Vaccine coverage and determinants of incomplete vaccination in children aged 12–23 months in Dschang, West Region, Cameroon: a cross-sectional survey during a polio outbreak. BMC Public Health. 2015;15(1):630.
Ateudjieu J, Kenfack B, Nkontchou BW, Demanou M. Program on immunization and cold chain monitoring: the status in eight health districts in Cameroon. BMC Res Notes. 2013;6(1):101.
Yakum MN, Ateudjieu J, Walter EA, Watcho P. Vaccine storage and cold chain monitoring in the North West region of Cameroon: a cross sectional study. BMC Res Notes. 2015;8(1):145.
Yauba S, Sobngwi J, Jude N, Tracy B, Kobela M, Charles N, et al. Temperature monitoring in the vaccine cold chain in Cameroon. J Vacc Vacc. 2017;1:09.
Yauba S, Harmelle EE, Marius VZ, Jude N, Delphine K, Calvin T, et al. Availability and status of vaccine cold chain equipment in Cameroon. J Vacc Vacc. 2019;10(2):1–6.
World Bank Group. Population, total-Cameroon|Data. 2021. Available from: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=CM.
Presidency of the Republic of Cameroon. Cameroon. Available from: https://www.prc.cm/en/cameroon.
Ministry of Public Health, Cameroon. Health Sector Strategy 2016–2027.
Wallace AS, Willis F, Nwaze E, Dieng B, Sipilanyambe N, Daniels D, et al. Vaccine wastage in Nigeria: An assessment of wastage rates and related vaccinator knowledge, attitudes and practices. Vaccine. 2017;35(48 Pt B):6751–8.
Uskun E, Uskun SB, Uysalgenc M, Yagız M. Effectiveness of a training intervention on immunization to increase knowledge of primary healthcare workers and vaccination coverage rates. Public Health. 2008;122(9):949–58.
Siddiqui FA, Padhani ZA, Salam RA, Aliani R, Lassi ZS, Das JK, et al. Interventions to improve immunization coverage among children and adolescents: a meta-analysis. Pediatrics. 2022;149(Supplement 6):e2021053852D.
Kanagat N, Krudwig K, Wilkins KA, Kaweme S, Phiri G, Mwansa FD, et al. Health care worker preferences and perspectives on doses per container for 2 lyophilized vaccines in Senegal, Vietnam, and Zambia. Glob Health Sci Pract. 2020;8(4):680–8.
World Health Organization. Reducing Missed Opportunities for Vaccination (MOV). Available from: https://www.who.int/teams/immunization-vaccines-and-biologicals/essential-programme-on-immunization/implementation/reducing-missed-opportunities-for-vaccination-(mov).
Assi TM, Brown ST, Djibo A, Norman BA, Rajgopal J, Welling JS, et al. Impact of changing the measles vaccine vial size on Niger’s vaccine supply chain: a computational model. BMC Public Health. 2011;11(1):425.
World Health Organization. WHO Policy Statement: Multi-dose Vial Policy (MDVP)- Handling of multi-dose vaccine vials after opening. Geneva; 2014. Available from: https://apps.who.int/iris/bitstream/handle/10665/135972/WHO_IVB_14.07_eng.pdf;sequence=1.
Al-Salihi LG, Aakef IR, Al-Shuwaili SJ, ZakiHadi WM. Primary health-care staff barriers to immunization. Indian J Community Med. 2019;44(3):256–60.
Filia A, Bella A, D’Ancona F, Fabiani M, Giambi C, Rizzo C, et al. Childhood vaccinations: knowledge, attitudes and practices of paediatricians and factors associated with their confidence in addressing parental concerns, Italy, 2016. Euro Surveill. 2019;24(6):1800275.
Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34(52):6700–6.
Acknowledgements
Regional delegates and districts staff for facilitating the conduct of the study in their respective districts and regions and the facility staff for their collaboration.
Funding
This study was funded by Bill and Melinda Gates Foundation (BMGF); however the outcome of the study does not necessarily represent the views of BMGF.
Author information
Authors and Affiliations
Contributions
Conception and design: YS, JG, AA, NJM, VMZ; statistical analysis: VNA, NJM; initial draft preparation: YS, SCN, BMN, CM; review and editing: YS, NNE, NJM, VMZ, CM, VNA, DO, DO, AAN, JF, DD, OW, EM, SACC; supervision: YS, OW, JG, SACC, EM, RC. All authors read and approved the submission of the final article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in compliance with the Helsinki Declaration and all applicable national laws and institutional rules and has been approved by the author’s institutional review board. Ethical approval was granted by the Cameroon National Ethics Committee for Human Health Research.
Informed consent
Informed consent was obtained from all subjects involved in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Saidu, Y., Gu, J., Ngenge, B.M. et al. The faces behind vaccination: unpacking the attitudes, knowledge, and practices of staff of Cameroon’s Expanded program on Immunization. Hum Resour Health 21, 88 (2023). https://doi.org/10.1186/s12960-023-00869-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12960-023-00869-7