- Review
- Open access
- Published:
Approaches to locum physician recruitment and retention: a systematic review
Human Resources for Health volume 22, Article number: 24 (2024)
Abstract
A robust workforce of locum tenens (LT) physicians is imperative for health service stability. A systematic review was conducted to synthesize current evidence on the strategies used to facilitate the recruitment and retention of LT physicians. English articles up to October 2023 across five databases were sourced. Original studies focusing on recruitment and retention of LT’s were included. An inductive content analysis was performed to identify strategies used to facilitate LT recruitment and retention. A separate grey literature review was conducted from June–July 2023. 12 studies were retained. Over half (58%) of studies were conducted in North America. Main strategies for facilitating LT recruitment and retention included financial incentives (83%), education and career factors (67%), personal facilitators (67%), clinical support and mentorship (33%), and familial considerations (25%). Identified subthemes were desire for flexible contracts (58%), increased income (33%), practice scouting (33%), and transitional employment needs (33%). Most (67%) studies reported deterrents to locum work, with professional isolation (42%) as the primary deterrent-related subtheme. Grey literature suggested national physician licensure could enhance license portability, thereby increasing the mobility of physicians across regions. Organizations employ five main LT recruitment facilitators and operationalize these in a variety of ways. Though these may be incumbent on local resources, the effectiveness of these approaches has not been evaluated. Consequently, future research should assess LT the efficacy of recruitment and retention facilitators. Notably, the majority of identified LT deterrents may be mitigated by modifying contextual factors such as improved onboarding practices.
Introduction
The shortage of a sustainable and robust physician workforce is a significant healthcare issue across most of the world [1]. In regions that face persistent challenges in physician availability, the continuity of the healthcare system heavily relies on locum tenens (LT) physicians, commonly referred to as “locums”. These healthcare providers work in a temporary capacity to fill vacancies or provide coverage for permanent physicians [2, 3]. Their importance was highlighted during the COVID-19 pandemic as the lack of locums resulted in the suspension of hospital services and emergency department closures due to insufficient staffing [4].
Physician recruitment strategies primarily focus on filling permanent positions with minimal emphasis on attracting locum providers [5]. However, strategies aimed at facilitating the recruitment of permanent physicians may not effectively attract locums given fundamental distinctions in their employment preferences and priorities. LTs, for instance, are motivated by factors such as seeking greater autonomy, working part-time, transitioning into partial retirement, and supplementing income [6, 7]. Their attraction to working as a locum may be due to advantages including reduced administrative burdens, lower workplace stress, and flexibility for maintaining a desired work–life balance [6, 7]. Additional advantages include competitive salaries comparable to permanent positions without a long-term commitment, travel and accommodation stipends, subsidized malpractice insurance, and lower overhead expenses [6, 7].
Governments and communities invest substantial financial resources to attract locums in order to sustain healthcare service delivery [6, 8]. As such, existing research has investigated locum recruitment and retention factors [6, 7, 9, 10]. Despite the important role that locums play in sustaining operational healthcare systems, particularly during periods of health human resources strain, there is a lack of consolidated of evidence on the recruitment of LT physicians. Consequently, there is a need for the synthesis of current research on facilitators used in the recruitment and retention of LTs. This will serve to better inform the development of comprehensive, evidence-based recruitment guidelines tailored specifically to LT physicians. Therefore, this study systematically reviewed existing literature to identify and synthesize the approaches used to recruit locum physicians. Ensuing results will provide valuable guidance to policymakers and healthcare organizations, aiding in the development of evidence-based recruitment policies and practices to address the unique needs of locum physicians.
Methods
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [11]. This research protocol was registered in the PROSPERO database (CRD42022339666).
Search strategy
Between April 26th and April 27th, 2022 we performed a systematic search of the electronic databases Ovid MEDLINE, Cochrane Database of Systematic Reviews, PsycINFO, CINAHL and Web of Science-Core Collection. Examples of the medical subject headings (MeSH) applied include “Contract Services”, “Career Choice”, “Personnel Staffing and Scheduling”, “Personnel Loyalty” and “Physician Incentive Plans”. This initial search has since been followed by an updated search in October of 2023 prior to submission for publication. Keywords were used to collect non-indexed material and those terms not captured by MeSH, such as “locum”. No limits were applied to the searches. Articles not available in English were excluded. Secondary research (e.g., meta‐analyses, dissertations, systematic reviews, case reports, commentaries, grey literature) were excluded from the scholarly search. Reference lists of included studies were searched for additional articles. Details of the scholarly search strategy appear in Additional file 1: Appendix S1. This search strategy was developed in collaboration with a librarian and peer-reviewed by a second librarian.
Between June 12th and July 16th, 2023 we performed an iterative systematic hand-search of grey literature. This included public search engines (e.g., Google), grey literature repositories (e.g., OpenGrey), health care quality organizations, and data facilities across five countries, Canada, United States of America, United Kingdom, Australia, and India. Examples of the search terms and headings applied include “Locum”, “Contract”, “Temporary”, and “Locum Physician''. Search parameters were restricted to include only articles published in the year 1990 or later. For database searches information beyond the first 150 or 250 search results were not incorporated in the analysis. For full search histories please see Additional file 1: Appendix S3.
Selection and screening process
A modified version of the PICO (population, intervention, comparison, outcomes) framework was used (Table 1) [12]. We included original qualitative, quantitative or mixed-methods studies focused on recruitment and retention initiatives specific to locums in any country across clinical settings. There was variability in how studies defined locum physicians (Table 2). Articles focusing on recruitment and retention of non-locum physicians and healthcare workers without an MD designation (with the exception of medical students training in a MD programme) were excluded, including articles that combined both populations in which individual data for locums could not be extracted. Articles that exclusively incorporated the recruitment and retention of locums in the interpretive context such that locum recruitment and retention initiatives were not prospectively mentioned in the study framework or methodology were excluded.
Retrieved articles were managed using Covidence online systematic review software (Veritas Health Innovation, Melbourne, Australia). Two reviewers independently performed title and abstract screening for relevance. Full texts were then reviewed against eligibility criteria (Table 1). In both stages of screening, discussion was used to resolve disagreements. Remaining discrepancies were resolved by a third reviewer.
Data extraction and synthesis
Data extraction took place within Covidence using two independent reviewers. A template was developed and piloted for two studies to ensure reviewer agreement prior to utilization. Outstanding conflicts were resolved by a third author. Extraction parameters included study design, participant characteristics, context of locum assignment, and strategies used to recruit and retain locums. Two authors (NF and OM) performed an inductive content analysis to characterize recurring patterns of the locum recruitment and retention strategies discussed in each paper included in the systematic analysis. Following the identification of these strategies, they were grouped into broader, overarching themes relevant to LT recruitment and retention. Methodologic quality of each study was assessed using the Mixed Methods Appraisal Tool (MMAT) [13]; two authors (NF and OM) conducted the appraisal independently and any discrepancies in appraisal were resolved by discussion with a third author (EO). Authors of included studies were contacted if data were missing.
Results
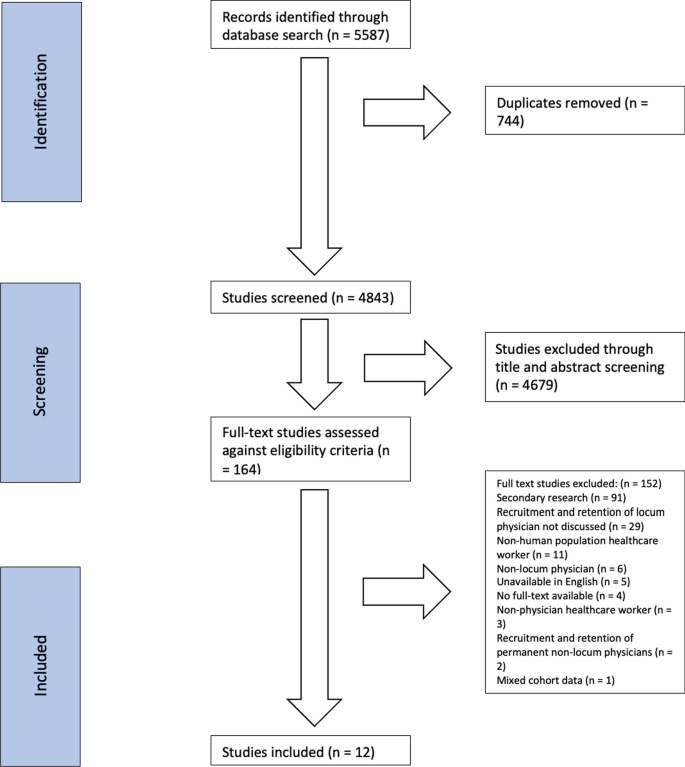
Our initial search identified 5390 citations. After the removal of duplicates (n = 812), 4578 studies’ titles and abstracts were screened. Following this stage, 242 articles were screened using full-text, and 230 were excluded from the review. Twelve studies [2, 3, 7,8,9, 13,14,15,16,17,18,19] fulfilled inclusion criteria and were retained for data extraction. The PRISMA flow diagram detailing the screening procedure is displayed in Fig. 1. Articles reporting data from the same participant population at separate time points are reported together.
Study characteristics are summarized in Table 3. Most (n = 11, 92%) studies [2, 3, 7,8,9, 13,14,15, 17,18,19] were published within the last 20 years of our search. Four (33%) studies [7, 9, 13, 19] were from the United States and four (33%) [8, 14,15,16] were from the United Kingdom. A smaller portion (n = 3, 25%) [2, 3, 17] originated in Canada. One (8%) study [18] was based in India. Quantitative studies [3, 7, 9, 13, 15,16,17] (n = 7, 58%) were cross-sectional (n = 6, 50%) [3, 7, 9, 13, 15, 16] or pre–post study (n = 1, 8%) [17] in design. Four (33%) studies [8, 14, 18, 19] used a qualitative design, including semi-structured interviews (n = 2, 17%) [18, 19], focus groups (n = 1, 8%) [14], and content analysis (n = 1, 8%) [8]. One (8%) study [2] adopted a mixed-methods design.
The majority of studies [2, 7,8,9, 13, 15, 16, 19] (n = 8, 67%) specified clinical setting, but did not indicate whether it was rural or urban (Table 3). A variety of specialities were reported among locum populations. The majority (n = 9, 75%) [2, 3, 7, 13,14,15,16, 18, 19] included primary care physicians, and over half (n = 5, 42%) [7, 9, 13, 18, 19] included specialists. Three (25%) studies [7, 13, 19] reported a subspecialist population. Two (17%) studies [2, 17] included physicians in training, with one (8%) [2] involving resident physicians and another (8%) [17] medical students. One (8%) study [8] did not indicate the specialty of the physician population. A total of six (50%) studies [7, 13,14,15,16, 19] reported years of physician practice experience.
A diversity of locum recruitment approaches were reported across studies, with some (n = 2, 17%) [7, 8] using more than one method. Four (33%) studies [7,8,9, 13] used a third-party recruitment agency, two (17%) [8, 14] used a locum bank, word-of-mouth, or personal networks [16], informal means [7], and an unspecified novel recruitment software were each reported once [8] (8%). Four studies [2, 15, 18, 19] (33%) did not report a specific method.
Quality assessment
The 2018 version of the MMAT was used to appraise the quality of retained articles [20]. Overall, nine (75%) of the articles [7, 8, 13, 14, 16,17,18,19] met 75–100% of the evaluated criteria, representing high quality. Three (25%) studies [2, 9, 15] met 50–75% of the evaluated criteria, representing moderate quality. Further details regarding the assessment of quality of retained articles appear in Additional file 1: Appendix S2. Grey literature was assessed using the AACODS Checklist [21]. Additional information on the appraisal of grey literature can be found in Additional file 1: Appendix S3 and in the supplemental content titled “Grey Literature Search Strategy, Data Extraction, and Evaluation”.
Facilitators of locum recruitment and retention
Six locum recruitment and retention themes were identified across retained studies (Table 4). Five overarching themes emerged for factors that facilitated LT recruitment and retention: financial incentives, familial considerations, educational or career-based factors, personal facilitators, and mentorship/clinical support. One theme focused on deterrents of locum work.
Ten (83%) studies [2, 3, 7,8,9, 13,14,15,16, 18] reported financial incentives with nine individual subthemes identified (Table 5). A significant portion (n = 4, 33%) of studies’ [2, 14,15,16] did not provide specific details about the nature of the financial incentives provided. Four (33%) of the studies’ [2, 7, 8, 13] financial incentives referred to an increase in income. Reimbursement for locum travel and lodging was reported three times (25%) [3, 7, 9]. Reimbursement for medical licensure (n = 2, 17%) and provision of malpractice insurance (n = 2, 17%) were also reported [7, 9]. Augmented pay for challenging work conditions [18], payment assistance for continuing medical education (CME) [18], supplementation of retirement income [13], and guaranteed income [3] were all reported once (8%) each.
Three (25%) studies [2, 7, 14] reported familial considerations as facilitators to recruitment and retention which included accommodating family (17%) [2, 14], school accessibility (8%) [14], and unspecified (8%) [7]. Furthermore, eight (67%) studies [2, 3, 7, 8, 13, 14, 16, 17] reported education or career-based incentives. A total of 13 subthemes related to educational and career-based factors facilitating recruitment and retention were reported (Table 5), which included pre-permanent practice scouting [2, 7, 13, 17] and temporary or transition in employment [2, 7, 13, 16] both reported four (33%) times. Freedom from administrative responsibilities and transitioning into retirement were reported three (25%) times [7, 13, 16]. Avoiding commitment [2, 16], increasing skills and competencies [2, 8], and a desire to take on part-time employment [7, 13] was reported twice (17%). The remaining career-based facilitators to recruitment and retention were each reported once (8%), including acquiring cross-provincial locum medical licensure [3], facilitation of hospital credentialing and medical licensure [7], gaining exposure to running a medical practice [2], accessing novel CME opportunities [3], assistance with maintaining medical knowledge [14], and accessing peer-facilitated educational support [14].
A total of eight (67%) studies [2, 7, 8, 13,14,15,16,17] reported using personal factors as facilitators of LT recruitment and retention. Within this category, five subthemes were identified (see Table 5). Seven (58%) reported using flexible contracts (e.g., suitable availability, work schedule flexibility, and work–life balance) [2, 7, 8, 13,14,15,16]. Having the ability to travel and experience new communities (locum tourism) was reported five (42%) times [2, 7, 13, 16, 17]. Three (25%) studies [7, 14, 15] reported unspecified personal incentives including stress relief [14], structured support [14], facility amenities [7], working conditions [7], personal safety [15], and overall facility quality [7]. Compatibility with post and convenience of the assignment were reported once (8%) each [8].
Four (33%) studies [14,15,16, 19] reported recruitment and retention facilitators involving mentorship and clinical support with four subthemes. Having a network of supportive colleagues [14, 15] and a chance to become familiar with the practice before arrival [16, 19] were reported twice (17%) each. Intentional relationship building, whereby the seasoned colleague met with the incoming locum to ensure comfort in the practice was reported once (8%) [19]. Availability of a back-up physician for support was reported once (8%) [19].
A total of eight (67%) studies [2, 8, 9, 14, 16,17,18,19] addressed deterrents of or barriers to locum work, encompassing a total of 19 reported subthemes. Professional isolation (n = 5, 42%) [2, 8, 14, 18, 19] was reported most frequently followed by work unpredictability (33%) [2, 8, 16, 19]. Insufficient patient continuity of care was reported three (25%) times [2, 8, 16]. The following deterrents/barriers were each reported twice (17%): inadequate employee onboarding and orientation [8, 19], demanding locum work [2, 17], poor job security [16, 18], lack of information to make an informed decision about accepting the job post [8, 9], and a lack of career advancement [16, 18]. The following deterrents/barriers were reported just once (8%): excessive travelling [16], low patient volume [2], administrative burden [18], difficulty accessing time-off [18], inadequate housing [18], challenging working conditions [18], exclusion from pension plans [16], lack of equitable pay [18], low salary [18], feeling distanced from CME and limitations in staying up-to-date [14], and perceptions of inferior professional status by colleagues [16].
Facilitators of locum recruitment and retention within grey literature
Grey literature findings closely mirrored the facilitators and deterrents found in peer-reviewed literature. A notable exception captured in the ‘education and career’ theme involved the potential benefits of implementing a national physician licensure, which was absent in the primary literature but present in nearly a third (n = 27, 26%) of the grey literature.
Interpretation
We identified 12 English language studies that explored the recruitment and retention of locums in Canada, USA, UK, and India over a 30-year period. Finance, education, and personal factors were the most used LT recruitment strategies while family considerations and clinical/mentorship support were less frequently cited. However, almost all studies [2, 3, 7, 8, 13,14,15,16] (n = 8, 67%) reviewed reported using a combination of these recruitment approaches. While there is a paucity of evidence on whether employing multiple approaches leads to improved LT recruitment, utilizing a range of methods may still be a reasonable strategy. This approach prevents organizations from becoming overly reliant on a single approach and enables them to adapt their strategy more easily as required to maintain LT recruitment, retention and service. Further, as physicians choose locum positions based on different priorities, utilizing multiple strategies provides a range of incentives with wider appeal.
Across the five LT recruitment strategies, the diverse range of unique approaches used indicates there is no one-size-fits-all method. This suggests that organizations develop their own specific approach tailored to their available resources, location, and the anticipated needs of the LT physicians they aim to recruit. For instance, certain recruitment strategies incentives such as back-up availability, network of supportive colleagues and access to CME may not be feasible for some organizations given their size, location, and resource constraints. This may lead to the development of alternative recruitment approaches and/or increased emphasis on other strategies. Notably, we found that common recruitment and retention strategies used elsewhere, such as providing competitive salaries, were extensively used in the recruitment and retention of locums. However, approaches that seem to be specifically designed to address the unique requirements and preferences of locum physicians were also employed, such as offering reimbursements for travel and accommodation, providing support for family-related needs, offering flexible scheduling, and facilitating access to leisure activities. Although the effectiveness of these strategies is poorly defined, their implementation suggests that organizations recognize that conventional recruitment and retention approaches, effective in the broader health workforce, may not adequately address the unique aspects and challenges associated with the transient and temporary nature of locum work. For example, incentives like competitive compensation, while valued, might not be as appealing to those seeking the flexibility of short-term work assignments or lifestyle benefits. Therefore, acknowledging the appeal of locum work, creating incentives that emphasize these benefits, and addressing the related challenges are likely to enhance recruitment and retention efforts.
The finding that showed sites employed a wide range of recruitment and retention approaches highlights the complexity of this process. However, implementing such a wide range of strategies makes it challenging to identify the most effectives. Consequently, future work should identify optimal recruitment strategies within diverse health contexts and organizational structures. This would enable organizations to streamline their approach, maximizing recruitment success while efficiently utilizing their resources. This may be particularly valuable in resource poor healthcare environments where strategic asset allocation is essential.
Numerous factors were cited as deterrents of locum work, indicating that physicians’ decision to work as a LT is influenced by a variety of considerations. Although some of the cited deterrents were addressed by recruitment strategies, it is unclear whether these approaches were effective. In the studies reviewed, professional isolation and work assignment predictability were the two most cited deterrents to locum work appearing in 42% and 33% of studies, respectively. As temporary workers, there are inherent challenges in developing rapport with colleagues. Moreover, providing coverage introduces uncertainties regarding work schedules and conditions (e.g., hours worked, frequency and duration of assignments). Together these factors can contribute to lower job satisfaction, which may result in a decreased willingness to work as a locum. As a result, recruitment strategies should consider measures to address these deterrents. The wide range of deterrents emphasizes the importance for healthcare organizations to adopt comprehensive recruitment strategies that recognize and respond to the various unique needs of LT physicians. Further, many of these deterrents may be addressed by improving locum onboarding and job conditions, such as enhancing infrastructure quality and minimizing social isolation.
It is important to recognize information on locum recruitment and retention extends beyond peer-reviewed articles to include the grey literature. These non-academic resources contain potential insights into practical approaches for recruitment and retention, thus underscoring the need to evaluate the grey literature in this field. Interestingly, our review of the grey literature generally aligns with the facilitators and deterrents of locum work identified in this systematic review apart from support for a national physician license. Such a measure would enhance the portability of licensure, allowing improved mobility of physicians across regions, reducing administrative burdens and the time required for obtaining proper licensing, hospital privileges, and contractual agreements. This, in turn, may reduce barriers to locum recruitment and more effectively facilitate the transition of locums to their temporary place of practice. This finding, which was not identified in the systematic review, again reiterates the importance of assessing the grey literature to gain a comprehensive understanding on the current strategies being used for recruiting and retaining locum physicians.
Importantly, the success of LT physician recruitment relies on a collaborative effort that extends beyond responsibility of individual healthcare organizations. This is particularly important considering that facilitators of LT recruitment and retainment, such as remuneration, fall beyond the scope of health teams. Therefore, the various stakeholders in health human resources, including educational institutions, regulatory bodies, and professional associations, all play a role in LT recruitment efforts. Recognizing and embracing this shared responsibility will be crucial in fostering a robust and sustainable healthcare workforce that incorporates LT physicians.
Limitations
In the systematic and grey literature reviews, a comprehensive set of keywords related to locum recruitment and retention were used (as detailed in Additional file 1: Appendices S1 and S3). However, some search terms, such as region-specific terminology used to describe locums, were not included. As a result, it is possible that relevant resources may have been missed during the literature search. However, the use of diverse keywords related to locum recruitment and retention would have captured relevant studies thus reducing the likelihood that relevant resources were missed. As described in the literature search strategies, date limitations were applied to both the systematic and grey literature searches, and only select databases were searched. Therefore, there is a possibility that relevant publications or grey literature produced outside of these date ranges or databases might have been missed. The quality of synthesized evidence was moderate as most of the retained quantitative studies were cross-sectional [3, 7, 9, 13, 15, 16] (50%) or mixed-methods [2] (8%). Only one study adopted a pre–post study design [17], which is fraught with internal validity issues. Remaining studies [8, 14, 18, 19] were qualitative and not inherently generalizable to broad populations. None of the studies were intervention-based, making it difficult to draw conclusions about the effectiveness of various recruitment and retention strategies. Inconsistent reporting on locum (LT) gender limited conclusions regarding differences in motivations for LT practice. Geographies of included studies reported were likely influenced by the methodological choice to include English only articles, limiting the generalizability of the presented findings to other regions. Further, the mix of qualitative and quantitative sources make it challenging to comprehend the cumulative size of the physician population raising each issue, and the relative significance of each issue compared to others.
Conclusions
This systematic review synthesized existing knowledge pertaining to international locum physician recruitment and retention strategies. Locum physicians are essential to the delivery of quality healthcare services across Canada and other parts of the world. We demonstrate that organizations employ five main LT recruitment strategies and deploy these in a variety of ways. Though these may be incumbent on local resources, more concerning is that the effectiveness of these approaches has not been tested. Given the present financial challenges within the global healthcare landscape there is a need to better understand recruitment and retention strategies of LTs so this limited resource can be used most effectively. Findings merit future research into the effectiveness of LT recruitment approaches via prospective methodologies.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Li JH, Scott A, McGrail M, Humphreys J, Witt J. Retaining rural doctors: doctors’ preferences for rural medical workforce incentives. Soc Sci Med. 2014;121:56–64.
Myhre DL, Konkin J, Woloschuk W, Szafran O, Hansen C, Crutcher R. Locum practice by recent family medicine graduates. Can Fam Physician. 2010;56(5):E183–90.
Rourke JTB, Incitti F, Rourke LL, Kennard MA. Keeping family physicians in rural practice—solutions favoured by rural physicians and family medicine residents. Can Fam Physician. 2003;49:1142–9.
Duong D. Why are emergency departments closing? Can Med Assoc J (CMAJ). 2022;194(33):E1138–9.
Abelsen B, Strasser R, Heaney D, Berggren P, Sigurðsson S, Brandstorp H, et al. Plan, recruit, retain: a framework for local healthcare organizations to achieve a stable remote rural workforce. Hum Resour Health. 2020;18(1):63–63.
Ferguson J, Tazzyman A, Walshe K, Bryce M, Boyd A, Archer J, et al. “You’re just a locum”: professional identity and temporary workers in the medical profession. Sociol Health Illn. 2021;43(1):149–66. https://doi.org/10.1111/1467-9566.13210.
Alonzo AA, Simon AB. Have stethoscope, will travel: contingent employment among physician health care providers in the United States. Work Employment Soc. 2008;22(4):635–54.
Theodoulou I, Reddy AM, Wong J. Is innovative workforce planning software the solution to NHS staffing and cost crisis? An exploration of the locum industry. BMC Health Serv Res. 2018;18:1–13.
DiMeglio M, Furey W, Laudanski K. Content analysis of locum tenens recruitment emails for anesthesiologists. BMC Health Serv Res. 2018;18:1–7.
Waldie AC. Put out the welcome mat for locums. Can Med Assoc J (CMAJ). 1998;158(8):1009–1009.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906–105906.
Larkin J, Foley L, Smith SM, Harrington P, Clyne B. The experience of financial burden for people with multimorbidity: a systematic review of qualitative research. Health Expect. 2021;24(2):282–95.
Simon AB, Alonzo AA. The demography, career pattern, and motivation of Locum tenens physicians in the United States. J Healthc Manag. 2004;49(6):363–75.
Jenson CM, Hutchins AJ, Rowlands G. Is small-group education the key to retention of sessional GPs? Educ Prim Care. 2006;17(3):218–26.
Jenson C, Reid F, Rowlands G. Locum and salaried general practitioners: an exploratory study of recruitment, morale, professional development and clinical governance. Educ Primary Care. 2008;19(3):285–302. https://doi.org/10.1080/14739879.2008.11493685.
McKevitt C, Morgan M, Hudson M. Locum doctors in general practice: motivation and experiences. Br J Gen Pract. 1999;49(444):519–21.
Woloschuk W, Tarrant M. Does a rural educational experience influence students’ likelihood of rural practice? Impact of student background and gender. Med Educ. 2002;36(3):241–7.
Rajbangshi PR, Nambiar D, Choudhury N, Rao KD. Rural recruitment and retention of health workers across cadres and types of contract in north-east India: a qualitative study. WHO South East Asia J Public Health. 2017;6(2):51–9.
Lagoo J, Berry W, Henrich N, Gawande A, Sato L, Haas S. Safely practicing in a new environment: a qualitative study to inform physician onboarding practices. Jt Comm J Qual Patient Saf. 2020;46(6):314–20. https://doi.org/10.1016/j.jcjq.2020.03.002.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed methods appraisal tool (MMAT), version 2018; 2018.
Tyndall J. AACODS checklist. Flinders University; 2010. https://www.library.sydney.edu.au/research/systematic-review/downloads/AACODS_Checklist.pdf
Acknowledgements
We gratefully acknowledge the help of Jennifer Dumond, Education Services Librarian at NOSM University, for peer-reviewing the search strategy.
Funding
Supported by Northern Ontario Academic Medicine Association (NOAMA) Academic Funding Plan (AFP) Innovation Fund Project #A-22-07.
Author information
Authors and Affiliations
Contributions
N.F and O.M were responsible for experimental design, the acquisition, analysis, interpretation of data and writing of the manuscript. A.C was responsible for acquisition, analysis, interpretation of data. I.R.L was responsible for interpretation of data, and the writing and revising of the manuscript. L.D and E.O were responsible for conception and experimental design, data analysis, data interpretation and revising the manuscript. All authors approve of the final version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All persons designated as authors qualify for authorship, and all those who qualify for authorship are listed.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Appendix S1
: Search Strategy. Appendix S2: Mixed-methods Appraisal Tool (MMAT) quality assessment of included studies. Appendix S3: Grey Literature Search Strategy, Data Extraction, and Evaluation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ferreira, N., McKenna, O., Lamb, I.R. et al. Approaches to locum physician recruitment and retention: a systematic review. Hum Resour Health 22, 24 (2024). https://doi.org/10.1186/s12960-024-00906-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12960-024-00906-z